Clinical highlights – March 2024
We are thrilled to inform you about the clinical benefits of eye tracking. Every once in a while, we keep you updated on the latest news shared by the scientific community.
The current newsletter will make you discover 3 recent articles highlighting the relevance of eye tracking for
- Concussion
- Alzheimer’s disease
- Parkinson’s disease.
Enjoy the read!
The neuroClues® Team
Automating the analysis of eye movement for different neurodegenerative disorders
Researchers from the John Hopkins Hospital developed a multi-task rapid battery test in a cohort encompassing multiple neurodegenerative disorders including mild cognitive impairment (MCI), Alzheimer’s disease (AD), Parkinson’s disease (PD), Parkinson’s disease mimics (PDM), and controls (CTRL).
The automated eye tracking analysis algorithms can extract interpretable and quantified biomarkers to evaluate the performance in smooth pursuit, saccade, visual exploration, and passage reading.
An example of sequences of screens for the five tasks employed along the timeline can be seen below.
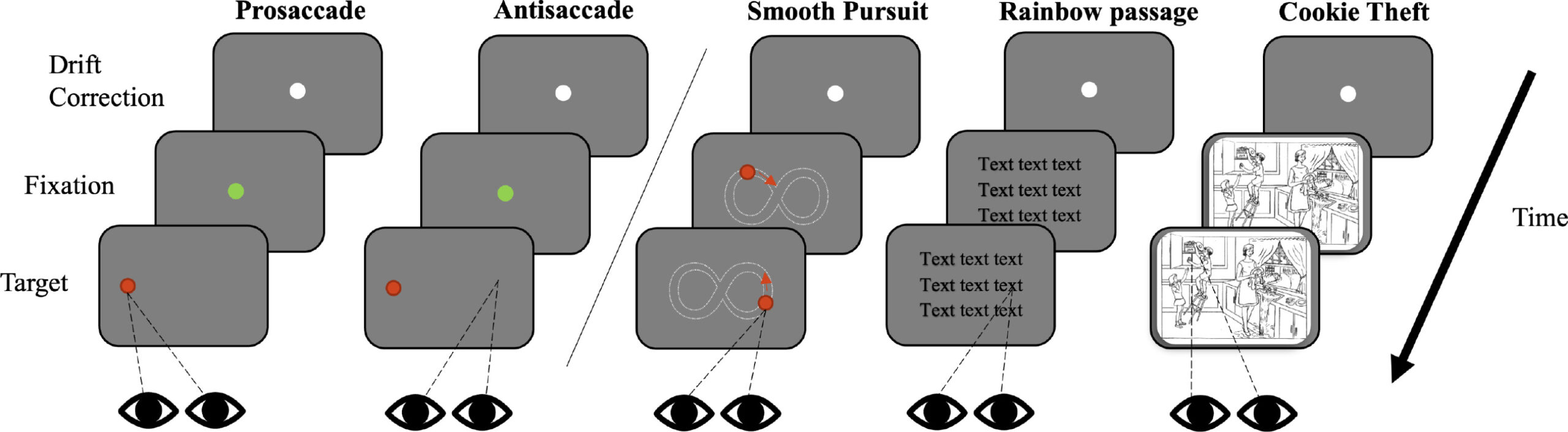
“In our case, five tasks (36 trials in total) were used, which took under 15 min to complete in a multi-modal multi-test rapid battery”
“These features, as oculographic biomarkers, can be potentially leveraged in distinguishing different types of NDs, yielding more objective and precise protocols to diagnose and monitor disease progression.”
Li et al. (2024)
Automated Eye Tracking Enables Saccade Performance Evaluation of Patients with Concussion History
A recent study in Optometry and Vision Science sheds light on saccade performance in 115 patients with a concussion history.
They reported that patients with concussion, on average, had fewer fixations on self-paced horizontal and vertical saccade tests and lower horizontal and vertical saccade speed/accuracy ratios compared with normative ranges.
They additionally identified risk factors for lower saccade performance among patients with a concussion history such as age, sex, number of concussion(s), and time from most recent concussion to oculomotor testing.
Future research could explore how the oculomotor performance changes over time, which may aid in ‘return-to-play’ decision-making for patients with sport-related concussion history.
“These findings support the use of saccade test results as biomarkers for concussion and have implications for post-concussion rehabilitation strategies.”
Song et al. (2023)
Eye Movement Study in Posterior Cortical Atrophy: A Case Report
In a recent case study, researchers used Video-Oculography to assess eye movements in a 64-year-old male with word-finding difficulties and mild visual spatial disturbances. They discovered marked increases in saccade latencies as seen in the table below, indicating dysfunction in the posterior parietal cortex. Subsequent investigations confirmed a diagnosis of posterior cortical atrophy (PCA) due to Alzheimer’s disease.
Eye movement studies have shown promise in distinguishing PCA from typical Alzheimer’s Disease, often revealing increased saccadic latencies and shorter saccades.
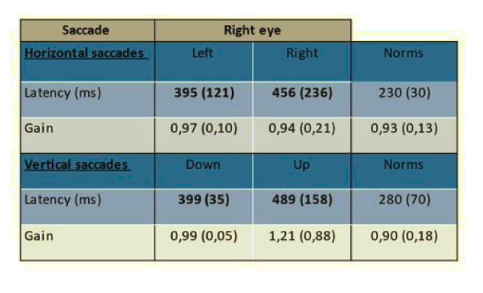
“… the case M.A. suggests that VOG may be impaired in the early stage of PCA and that its diagnostic value relative to imaging and cognitive assessment needs to be assessed in future studies”
Pin et al. (2023)