Clinical highlights – August 2024
We are excited to share insights into the potential of eye tracking. Every month, we keep you updated on the latest news shared by the scientific community.
The current newsletter will emphasize the latest research about Multiple Sclerosis (MS) and the view of clinical experts on the relevance of eye-tracking for this diseases.
Enjoy the reading!
The neuroClues® Team
Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic inflammatory neurological disorder characterized by the immune system mistakenly attacking the protective covering of nerve fibers in the central nervous system, leading to communication disruptions between the brain and the rest of the body. This can result in various symptoms, such as coordination and balance difficulties, movement disorders, and issues with vision and cognition, with fatigue further exacerbating these symptoms.
It impacts approximately 2.8 million individuals globally.
MS can affect any part of the central nervous system. Since eye movement circuits span various brain regions, they may overlap with MS-affected areas. This prompted researchers to explore the topic.
The clinical classifications of MS are:
- Relapsing-Remitting MS (RRMS): Characterized by flare-ups (relapses) of symptoms followed by periods of improvement or stability (most common)
- Secondary-Progressive MS (SPMS): Often follows RRMS. Symptoms progressively worsen over time, with fewer or no relapses.
- Primary-Progressive MS (PPMS): Affects about 10% of MS patients, with a steady worsening of symptoms from the beginning, without relapses.
- Progressive-Relapsing MS (PRMS): A rare form where symptoms steadily worsen from the onset, with intermittent relapses.

About 18% of people diagnosed with MS may not have the disease.
One study found that 50% of misdiagnosed patients carried the incorrect diagnosis for at least three years, and 70% received disease modifying-therapy for a disease they didn’t have.
Diagnosing MS
Assessing MS involves a combination of clinical evaluation, neurological examination, MRI scans to visualize lesions in the central nervous system, and other tests to rule out other possible causes. MS diagnosis relies on the demonstration of lesions disseminated in space and time, meaning evidence of damage in multiple parts of the central nervous system occurring over time. Clinicians use the McDonald Criteria, which have been revised several times (most recently in 2017), to standardize the diagnostic process.
Challenges in diagnosing
Assessing MS can be difficult due to its diverse symptoms and unpredictable disease progression. Current treatments are often limited, especially for the progressive forms of MS. Additionally, clinicians distinguish between two types of MS: inflammatory and degenerative. This distinction is crucial because, while we have effective treatments for inflammatory MS, there are no therapies for the degenerative form, which adds to the complexity of managing the disease.
Eye movement analysis could offer a high clinical utility while being supported by the most scientific evidence.
More information can be found on our science webpage.
Ophthalmic Biomarkers are Emerging as a Promising Tool for Evaluating MS Progression
New research is focusing on non-invasive techniques, including oculomics, which studies ocular manifestations related to systemic diseases. This includes analyzing changes in the retina and optic nerve, which are directly linked to brain health, as well as novel biomarkers in ocular fluids and eye-tracking movements.
There are two common saccadic disorders observed in patients with MS:
I. Ophtalmoparésie Internucléaire (INO)
INO occurs due to the demyelination of nerve fibers in a specific brain region called the medial longitudinal fasciculus (MLF) located in the pons. When the signals are disrupted, it leads to a condition where the eye that is supposed to move inward (adducting eye) does so more slowly than the eye moving outward (abducting eye) during horizontal saccades. This miscoordination is termed as adduction lag.
INO can be assessed by comparing the peak saccade velocities of the abducting and adducting eyes, with studies showing that patients with INO have higher peak velocities in the abducting eye than healthy individuals.These measurements can help gauge the severity of MS and may correlate with MRI findings of abnormalities in the MLF.
Indeed, INO can be clinically observed as dissociated nystagmus in the abducting eye. However, incorporating eye tracking into consultations can detect INO at earlier stages, even when it is not visible to the naked eye. Eye tracking also provides objective measurements of INO and tracks its progression over time with different treatments.
II. Saccadic Dysmetria
It is caused by lesions in the cerebellar peduncles. These lesions impair the smooth pursuit movements and the ability to suppress the horizontal vestibulo-ocular reflex (VOR), which is essential during tasks that require tracking moving objects with combined eye-head movements.
Saccadic dysmetria can present as gaze-evoked nystagmus (GEN) or downbeat nystagmus (DBN), each linked to specific neural deficits. GEN results from a defect in the neural integrator network, while DBN is due to loss of inhibitory control by the cerebellum on the vertical semicircular canals.
This paper highlights the potential of eye-tracking technology as a non-invasive tool for objectively quantifying saccadic disorders, which can assist in early diagnosis, monitoring disease progression, and evaluating treatment response in MS patients.
Evidently, tracking of dysmetria and saccadic eye movements demonstrates prognostic potential for evaluating the severity of MS as well as the therapeutic effect of various treatments
(…)
Paired with machine learning, researchers may enhance the diagnostic accuracy of saccadic eye movements with VR and open new insights on the functional and oculomotor visual markers throughout disease progression.
Suh et al., 2024
Why is early diagnosis and disease monitoring important ?
Early diagnosis and monitoring of Multiple Sclerosis (MS) are crucial for initiating timely treatment (e.g. disease-modifying therapies), delaying disease progression, reducing relapse rates, and improving long-term outcomes. Additionally, accurate early diagnosis also differentiates MS from other conditions, preventing unnecessary investigations and inappropriate treatments.
Using the McDonald criteria, clinicians can distinguish between Clinically Isolated Syndrome-CIS (with observable MS symptoms) and Radiologically Isolated Syndrome-RIS (detected on MRI without clinical signs). However, it remains unclear whether patients with RIS are truly asymptomatic or if their symptoms are simply too early to detect. Eye movement analysis could provide valuable insights into these subtle, non-clinical symptoms, leading to more precise diagnoses.
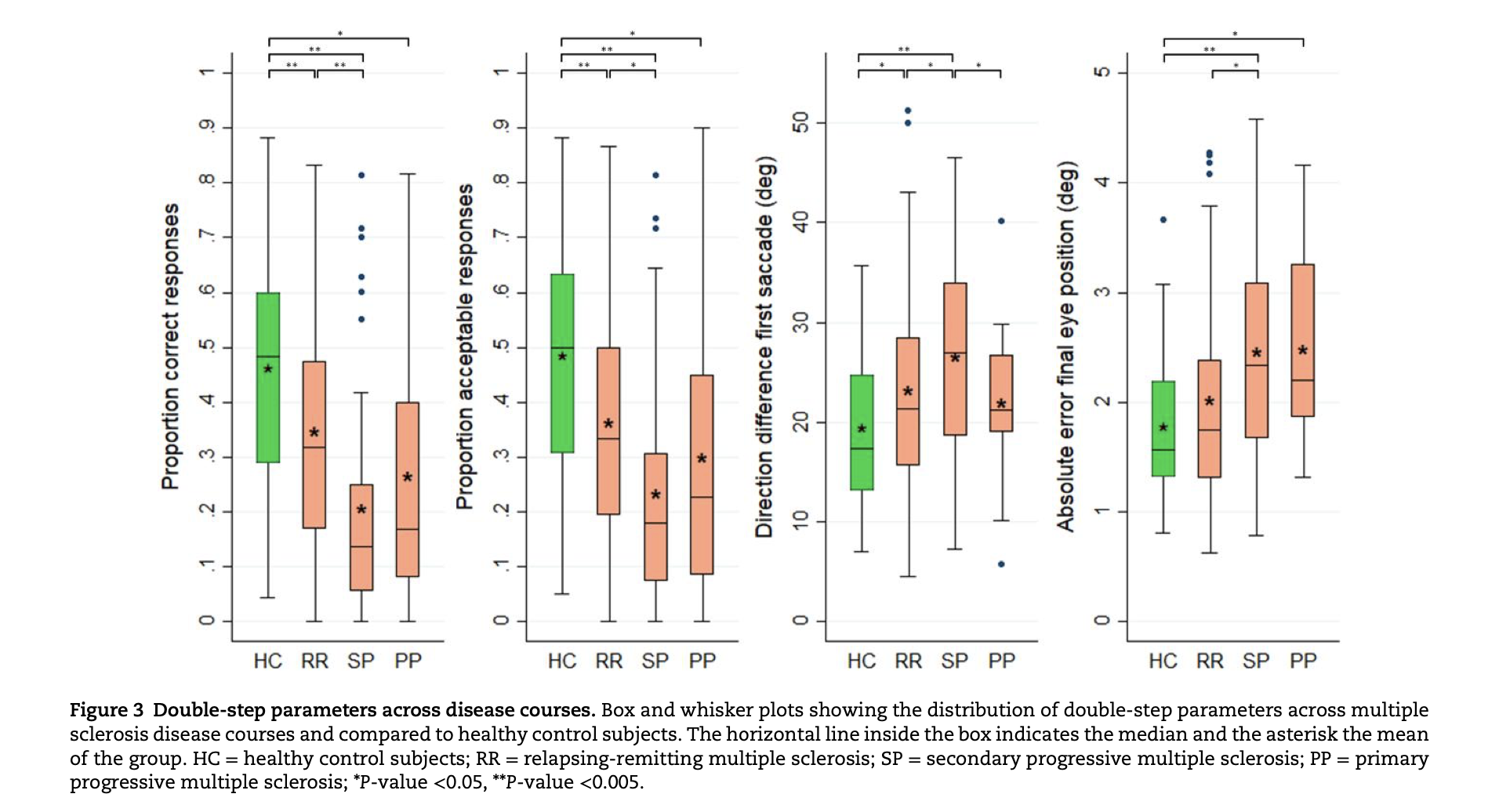
Double-step saccadic test to enhance MS assessment
The double-step saccadic test requires executing two rapid saccades towards sequential stimuli, engaging multiple cortical and subcortical networks. This complexity makes it a more sensitive indicator of cognitive and motor function than simpler tasks like single-step saccades. It can detect subtle changes in eye movement control, offering a nuanced view of disease progression or treatment response in multiple sclerosis.
The study demonstrates that the double-step saccadic test has stronger statistical correlations with clinical, cognitive, and MRI metrics compared to traditional saccadic tests. For instance, individuals with multiple sclerosis showed a significantly lower proportion of correct double-step saccades compared to healthy controls, with these results correlating with grey matter atrophy, lesion load, and cognitive impairments.
Proposed as a novel outcome measure for remyelination trials, the double-step saccadic test offers a promising alternative for assessing treatment efficacy by reflecting both structural damage and cognitive function, addressing a key limitation of many traditional eye movement assessments.
Enjoyed this article?
Join our community to receive a monthly newsletter featuring insights on the relevance of eye tracking in the clinic and exclusive company updates