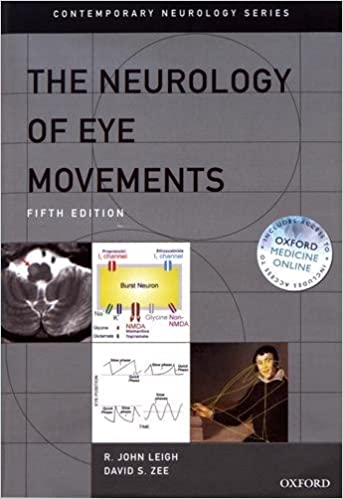
Our inspiration
Over the last 60 years, over 110.000 scientific articles have been written linking eye movements with the neural area that commands them, and ultimately their link with neurological diseases.
These findings have been thoroughly described in R. John Leigh and David S. Zee’s The Neurology of Eye Movements. Their book in two parts provides
- a synthesis of the characteristics of eye movements based on the study of macaques and humans and
- their applications to the analysis of patients with abnormal eye movements.
In other words, there is a wealth of knowledge on the typical saccade, fixation, poursuit and pupillometric characteristics of healthy and pathological subjects.
Practical applications
Today, this wealth of scientific knowledge can be used in consultation to help the practitioners quantify their clinical examination. We list here one of many examples for each field of application:
Early stage diagnosis
Recent studies have identified antisaccades latency as a predictive biomarker to identify the subpopulation of Parkinson patients who will develop freezing of gait, up till 5 years in advance!
Antisaccade latency is a predictive marker of the 5-year onset of freezing of gait
Saccade abnormalities are clearly different in SND, CBD, and PSP, and might help in early differential diagnosis in individual patients
Differential diagnosis
Maybe one of the best know examples of the discrimination based on eye movements, is the diagnosis of Progressive Supranuclear Palsy from idiopathic Parkinson, based on a speed reduction of vertical saccades.
Follow-up
In Multiple Sclerosis, existing scales can be enhanced with the analysis of eye movements, as ocular motor manifestations are highly prevalent in MS, whereas chronic manifestations may cause minimal or no symptoms. Performed in the daily practice, this can inform a treatment adaptation and improve the visual outcome.
Appropriate treatment may improve visual outcome in some of these ocular motor disorders.
Why not in your clinical practice?
There are three reasons why eye tracking has not been widely implemented in the clinical practice to date.
It takes a highly qualified personnel
to operate eye trackers
and interpret the results.
Eye trackers are complex to use, often requiring a dedicate room, a cumbersome set up and a separate consultation.
Eye tracking devices are too expensive
for the practitioners,
to purchase and to operate.
These pains are our founders’ frustrations over 20 years of research on eye movements. We’re on a mission to answer those issues. That’s why we are developing NeuroCluesTM, a portable lab to help you instantaneously quantify your clinical exam, based on eye tracking.
The product is not yet available for sale and will soon undergo clinical investigations.
Sources :
John R. Leigh and David S. Zee, The Neurology of Eye Movements, Fifth edition, 2015, Contemporary Neurology Series
Cécile Gallea, Benoit Wicki, Claire Ewenczyk, Sophie Rivaud-Péchoux, Lydia Yahia-Cherif, Pierre Pouget, Marie Vidailhet, Elodie Hainque, Antisaccade, a predictive marker for freezing of gait in Parkinson’s disease and gait/gaze network connectivity, Brain, Volume 144, Issue 2, February 2021, Pages 504–514, https://doi.org/10.1093/brain/awaa407
Vidailhet, M., Rivaud, S., Gouider-Khouja, N., Pillon, B., Bonnet, A.-M., Gaymard, B., Agid, Y. and Pierrot-Deseilligny, C. (1994), Eye movements in parkinsonian syndromes. Ann Neurol., 35: 420-426. https://doi.org/10.1002/ana.410350408
- Nerrant E, Tilikete C. Ocular Motor Manifestations of Multiple Sclerosis. J Neuroophthalmol. 2017 Sep;37(3):332-340. doi: 10.1097/WNO.0000000000000507. PMID: 28410279.